For millennia, the human narrative was frequently truncated by the smallest of biological footnotes.
A simple dermal abrasion from a garden thorn or a localized infection was not merely a physical inconvenience; it was a primary driver of global mortality. Before the mid-20th century, the epidemiological landscape was defined by clinical helplessness. With life expectancy at birth hovering near just 47 years, outcomes were a primitive gamble between a patient’s innate immune response and the onset of systemic sepsis.
The paradigm shifted with a moment of scientific serendipity in 1928. Alexander Fleming’s observation of the bactericidal properties of the Penicillium notatum mold ushered in the antibiotic era, moving medicine from reactive palliation to active intervention. By inhibiting bacterial cell wall synthesis, this "miracle" compound effectively neutralized once-fatal pathogens, contributing to a profound demographic shift that added an estimated 20 years to the global average human lifespan.
Yet, we now face a period of "Great Adaptation." The selective pressure exerted by decades of antibiotic use has forged a new generation of highly resistant bacterial strains; an invisible army evolving to bypass the molecular mechanisms designed to destroy them. Statistical projections are stark: current data suggest that without the development of novel therapeutic classes, Antimicrobial Resistance (AMR) could claim 10 million lives annually by 2050, potentially eclipsing oncology as a leading cause of global mortality.
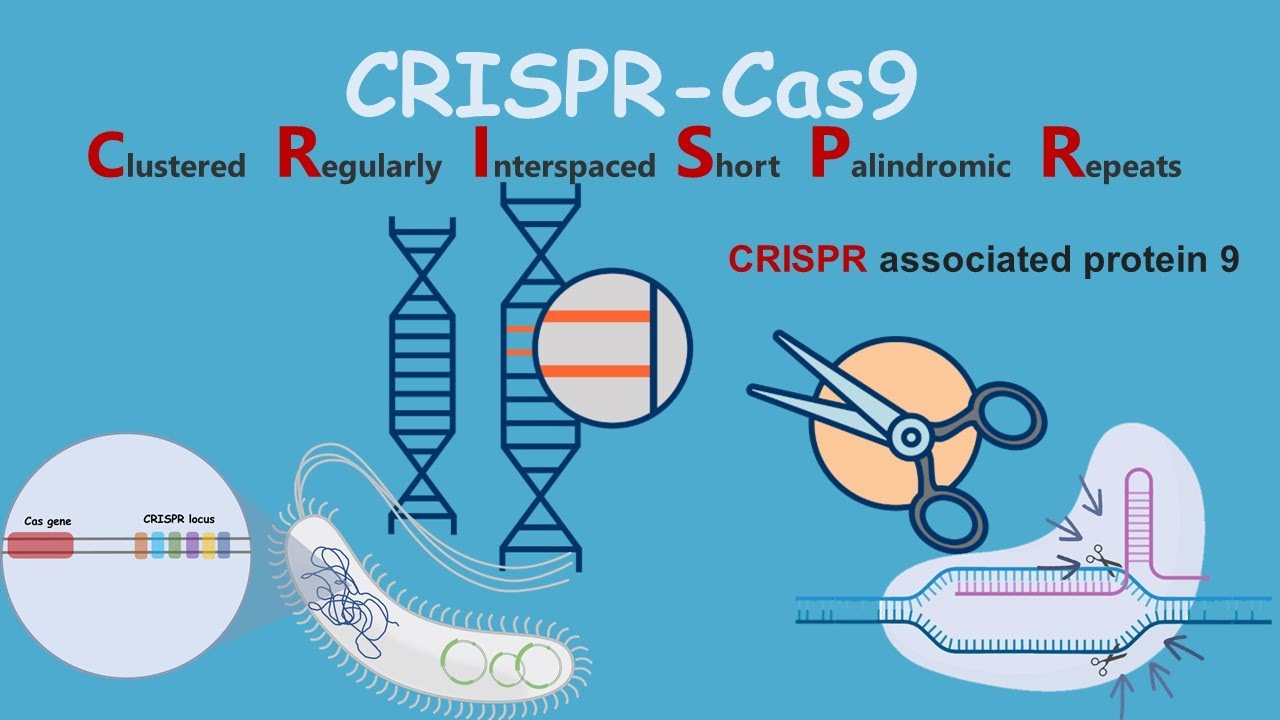
We are entering a new chapter where hope is no longer found in accidental spores, but is forged from silicon and code. We utilize Artificial Intelligence as a high-throughput scout, sifting through millions of chemical combinations in a single heartbeat to identify the one "needle in the haystack" molecule that can pierce modern bacterial armor. We are learning to edit the blueprints of our enemies using CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats), disabling virulence factors with surgical precision before they can cause harm.
In conclusion, the future of medicine is no longer a search for new "juices," but a mastery of biological entropy. As we deploy nanobots to deliver targeted therapies directly to the site of infection with a precision once thought impossible, we fulfill a centuries-old promise. We are ensuring that the smallest scratch remains exactly that: a minor detail in a long, healthy life, rather than the final period at the end of a short sentence.